Maximizando el impacto de los escasos recursos de prueba de COVID-19

por el Dr.. alison connor, Dr. brezo lanthorn, Nisha Hariharan, & sarah carson
![]() A more detailed version of this blog was originally published in IDeas, the IDinsight blog.
A more detailed version of this blog was originally published in IDeas, the IDinsight blog.
Testing capacity has expanded dramatically in many countries since the start of the COVID-19 pandemic. Además, a number of countries have implemented highly innovative strategies: Rwanda has a sophisticated test pooling system and is using robots to monitor some COVID-19 patients. En Ghana, drones are now transporting some testing samples. There are signs, Sin embargo, that these expansions in capacity and innovation are still insufficient to overcome undeniable shortages in testing capacity, including both the supply of test kits and the ability to efficiently process them, due to lack of human resources and lab capacity. In addition to low test volume, many health systems are also too slow in processing and communicating test results to meaningfully change behavior.
Back in April, IDinsight partnered with the Global Health Group at the University of California, San Francisco to form a Pandemic Response Initiative. We have worked closely with the Clinton Health Access Initiative (CHAI) to answer this question: What is the most optimal way for countries to efficiently allocate limited diagnostic resources? When operating with insufficient testing capacity, it is critical to have a systematic way to allocate constrained COVID-19 testing resources to the highest impact uses for epidemic management.
We propose that a high-impact test meets the following three criteria:
- Strong potential to contribute to epidemic management goals
- Results are most likely to drive impactful action
- A reduction in uncertainty about someone’s COVID-19 infection status
These three criteria form the backbone of the PRIoritize_Dx tool, our solution for a clear, actionable, and data-driven approach to support policymakers in effectively prioritizing their COVID-19 tests. The tool is interactive, allowing users to input key information about local conditions (such as isolation behavior, test turnaround time,) and receive tailored recommendations appropriate to their country context. We are currently piloting its use across a number of CHAI country offices across Sub-Saharan Africa and Asia.
Three criteria to optimize use of COVID-19 diagnostics
1. Dedicate tests toward the uses most likely to control the epidemic
As in other epidemics, el ultimate goal of any response effort to the COVID-19 pandemic is to reduce the overall morbidity and mortality in a population. Diagnostics are one key lever to achieving this goal, in addition to prevention and treatment. En particular, diagnóstico, when acted upon, contribute to this goal through four pathways:
- Reducing transmission: Diagnostics can inform behavior which can halt disease spread, breaking COVID-19 transmission and reducing new infections.
- Gaining information about disease burden: When policymakers have more granular testing data, they can understand the effectiveness of current mitigation strategies and channel support and resources where they are needed most.
- Determining optimal treatment for patients: Though no standardized COVID-19 treatment is widely available in LMICs, in the future, diagnostics could guide the use of these therapeutics.
- Maintaining the health system through testing frontline health care workers, who are essential for support testing and treating patients.
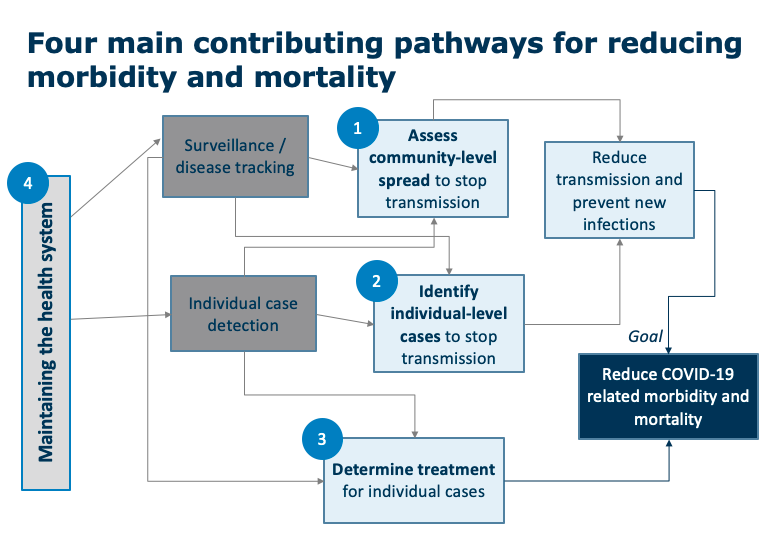
When laying out every possible use for a COVID-19 test, some uses are better positioned to contribute to these goals than others. Overall, we start by prioritizing the uses that are most obviously and directly linked to these four big-picture pathways for impact.
2. Prioritize tests when the results are most likely to drive impactful action
The first criterion was about a test’s potential contribution to epidemic goals; the second focuses on whether, given the context, this test will actually contribute to these goals based on its likelihood of driving action. This criterion is the most crucial of the three, because testing alone cannot achieve epidemic control if action does not follow. These actions may be at the individual level (por ejemplo. someone’s ability or willingness to isolate or access to improved care or treatment) or the community level (por ejemplo. localized lockdowns or changes in resource allocation). En última instancia, in resource-limited settings we should prioritize tests for situations when the results are most likely to be directly used.
3. Test when diagnostics will reduce uncertainty about a population’s COVID-19 status
Even if a test is highly relevant to epidemic management goals, and likely to trigger direct action, we must still ask ourselves whether this information must come from a test. While diagnostics are generally the most definitive information about someone’s COVID-19 status, a health care provider or policy-maker also considers the presence of symptoms, risk profile, likely exposure to confirmed cases, and the overall prevalence in the surrounding environment. In some scenarios, this other information provides a clear picture of someone’s likely status, meaning that a test result for this individual will not provide much new information. We should prioritize tests in contexts where our pre-existing level of uncertainty is the highest, and a test therefore has the greatest contribution to our knowledge base.
Putting the three criteria into action
COVID-19 testing resources are scarce, especially in LMICs. It is critical for decision-makers to carefully consider the optimal allocation of these resources in order to approach achieving epidemic control. These three criteria provide a framework to guide these challenging decisions. El PRIoritize_Dx tool supports LMIC policy-makers and public health advisors in applying this framework. This tool is designed to weigh these three criteria along with elements of a user’s COVID-19 response context to give highly tailored recommendations. The trade-offs vary across countries given differences in factors such as lab system capacity, the ability of community members to self-isolate, and the operational feasibility of different testing approaches (por ejemplo. contact tracing). But more broadly, we believe that these criteria are highly applicable for anyone involved in advising, implementar, or monitoring COVID-19 response in resource-limited settings. By ensuring that tests are prioritized for uses that are closely related to epidemic management goals, reduce uncertainty about someone’s COVID-19 status, and drive impactful action, policymakers can craft context-specific testing strategies that optimize the use of limited diagnostics.
The PRIoritize_Dx tool is now being rolled out and tested with CHAI, but we are seeking additional government partners interested in actively piloting this approach to testing and monitoring the results. For questions and comments, reach out our team at [email protected]
SOBRE LOS AUTORES
 Sarah Carson is a Senior Associate at IDinsight, based in Nairobi, Kenia. Prior to joining IDinsight, Sarah gained field research experience as a Youth, Migration, and Resilience Fellow with Save the Children, which involved managing a mixed methods data collection and analysis process focused on the livelihoods of young Ethiopian rural-urban migrants. Sarah has also served as a Peace Corps Volunteer in Rwanda, where she taught English at a secondary school and partnered with her community on efforts related to youth development, financial inclusion, and gender equality. Sarah holds a Master of Arts in Law and Diplomacy from the Fletcher School at Tufts University, with a focus on Development Economics and Business for Social Impact. She completed her Bachelor’s degree in International Affairs from the Honors Program at George Washington University.
Sarah Carson is a Senior Associate at IDinsight, based in Nairobi, Kenia. Prior to joining IDinsight, Sarah gained field research experience as a Youth, Migration, and Resilience Fellow with Save the Children, which involved managing a mixed methods data collection and analysis process focused on the livelihoods of young Ethiopian rural-urban migrants. Sarah has also served as a Peace Corps Volunteer in Rwanda, where she taught English at a secondary school and partnered with her community on efforts related to youth development, financial inclusion, and gender equality. Sarah holds a Master of Arts in Law and Diplomacy from the Fletcher School at Tufts University, with a focus on Development Economics and Business for Social Impact. She completed her Bachelor’s degree in International Affairs from the Honors Program at George Washington University.
 Nisha Hariharan is a Senior Manager at IDinsight based in Nairobi, Kenia. In her current role, Nisha is responsible for leading and executing engagements ranging from supporting government clients to test out accurate and efficient approaches for household-level data collection to working with community-health focused NGOs to implement improved evidence-driven methods for internal learning and innovation. Prior to joining IDinsight, Nisha served as a Program Manager for the Clinton Health Access Initiative’s (CHAI) eMTCT and Pediatric HIV team, managing a multi-country program to scale-up evidence-based interventions and policy across Sub-Saharan Africa. Nisha also worked as a consultant at Oliver Wyman focusing on providing analytical and strategic support to financial sector clients. Nisha holds a bachelor’s degree in Actuarial Science and Statistics (BMath) from the University of Waterloo, and a master’s degree in Global Disease Epidemiology (MSPH) and Control, from Johns Hopkins Bloomberg School of Public Health.
Nisha Hariharan is a Senior Manager at IDinsight based in Nairobi, Kenia. In her current role, Nisha is responsible for leading and executing engagements ranging from supporting government clients to test out accurate and efficient approaches for household-level data collection to working with community-health focused NGOs to implement improved evidence-driven methods for internal learning and innovation. Prior to joining IDinsight, Nisha served as a Program Manager for the Clinton Health Access Initiative’s (CHAI) eMTCT and Pediatric HIV team, managing a multi-country program to scale-up evidence-based interventions and policy across Sub-Saharan Africa. Nisha also worked as a consultant at Oliver Wyman focusing on providing analytical and strategic support to financial sector clients. Nisha holds a bachelor’s degree in Actuarial Science and Statistics (BMath) from the University of Waterloo, and a master’s degree in Global Disease Epidemiology (MSPH) and Control, from Johns Hopkins Bloomberg School of Public Health.
 Alison Connor is the Director of Health at IDinsight, based in Nairobi, Kenia. Alison leads IDinsight’s health strategy, identifying new opportunities in the health sector and providing expertise to health projects across all IDinsight offices. Previamente, Alison was based in Zambia with IDinsight for 2.5 años. Her past projects include a community-based cluster RCT on childhood immunization financial incentives in rural Nigeria, a learning partnership with the government of Ethiopia, and several demand-focused evaluations with the government of Zambia in both health and social protection. Alison was also a founding member of IDinsight’s technical team and has led internal training and professional development initiatives for the organization. Alison holds a BA in Government from Harvard University and a PhD in Global Disease Epidemiology and Control from Johns Hopkins Bloomberg School of Public Health.
Alison Connor is the Director of Health at IDinsight, based in Nairobi, Kenia. Alison leads IDinsight’s health strategy, identifying new opportunities in the health sector and providing expertise to health projects across all IDinsight offices. Previamente, Alison was based in Zambia with IDinsight for 2.5 años. Her past projects include a community-based cluster RCT on childhood immunization financial incentives in rural Nigeria, a learning partnership with the government of Ethiopia, and several demand-focused evaluations with the government of Zambia in both health and social protection. Alison was also a founding member of IDinsight’s technical team and has led internal training and professional development initiatives for the organization. Alison holds a BA in Government from Harvard University and a PhD in Global Disease Epidemiology and Control from Johns Hopkins Bloomberg School of Public Health.
 Heather Lanthorn is an Associate Director at IDinsight, based in the United States. Prior to joining IDinsight, Heather served as an Evaluation Specialist for the International Initiative for Impact Evaluation (3ie) and as a Research Associate at Innovations for Poverty Action (IPA) in Ghana. Her work at IPA focused on malaria medication completion in northern Ghana. She also interned in Advocacy, Communication and Social Mobilization with Stop TB in Geneva and was an Americorps VISTA volunteer with Habitat for Humanity in San Francisco. Heather holds a bachelor’s degree, cum laude and honors, in Anthropology with minors in Health Policy and Administration and Neuroscience from Wake Forest University. She also holds a Masters in Public Health (department of Health Behavior and Health Education) from the University of Michigan School of Public Health and a Doctorate of Science (health systems track in Global Health and Population department) from the Harvard T.H. Chan School of Public Health.
Heather Lanthorn is an Associate Director at IDinsight, based in the United States. Prior to joining IDinsight, Heather served as an Evaluation Specialist for the International Initiative for Impact Evaluation (3ie) and as a Research Associate at Innovations for Poverty Action (IPA) in Ghana. Her work at IPA focused on malaria medication completion in northern Ghana. She also interned in Advocacy, Communication and Social Mobilization with Stop TB in Geneva and was an Americorps VISTA volunteer with Habitat for Humanity in San Francisco. Heather holds a bachelor’s degree, cum laude and honors, in Anthropology with minors in Health Policy and Administration and Neuroscience from Wake Forest University. She also holds a Masters in Public Health (department of Health Behavior and Health Education) from the University of Michigan School of Public Health and a Doctorate of Science (health systems track in Global Health and Population department) from the Harvard T.H. Chan School of Public Health.




Respuestas